By Dhiraj Arora, as featured in Clinical Dentistry journal • January 2022
The concept here changes our focus to considering the structure, stability and integrity of the tooth and treating that before any endodontic work is undertaken. Instead of attending to the tooth structure afterwards, a really solid and common-sense approach is to use a little pre-endodontic build up magic at the outset.
Teeth that are subject to endodontic treatment generally demonstrate a distinctive loss of structure. This can be due to existing carious lesions, large fillings, fractures, bruxism or previous prosthetic restoration. The exception is traumatised teeth, which may not have been subject to dental treatment before the time of the accident.
An important building block in endodontic treatment is the use of a pre-endodontic build-up that creates an antibacterial seal, preventing further bacteria from the oral cavity getting into the pulp chamber and root canal system.
After anesthetizing the patient, the first step should be to isolate the affected region using a rubber dam. It’s advisable to use the rubber dam on the tooth to be treated – and also the neighbouring teeth. Only in this way is it possible to place a matrix cleanly. This in turn makes it possible to achieve the optimum isolation of the proximal contact point and ensure the filling fits the edges of the cavity walls precisely.
Another benefit of carrying out multiple teeth isolation is that it allows for improved orientation and the decisive shaping of the access cavity. Teeth that really can’t be isolated using a rubber dam should be subject to a critical examination to assess whether the tooth is actually restorable or not.
After positioning the rubber dam, all existing restorative materials must be removed. This and all other steps should take place ideally using magnification and, preferably, a dental microscope.

[Figure 1: Caries Indicator Dye for caries removal]
All carious hard tooth tissue structures must also be removed at this stage. Removing all carious lesions at this early stage of treatment is crucial as this is the only way to prevent reinfection of the pulp chamber system by the bacteria that cause caries. Using a caries detector dye can help clearly identify any existing areas (Fig 1).

[Figure 2: Caries removal endpoint with the presence of a palatal crack evident]
After this essential preparation work you can accurately assess the remaining tooth structure. It also allows for the discovery and assessment of any existing fracture lines. At this point you can classify the tooth in terms of its restorability (Fig. 2).
The presence of healthy tooth structure allows for the repair of the hard tooth tissue defects with a restoration that adheres to dentine and provides an antibacterial seal. This is crucial for all further steps in endodontic treatment and the creation of an effective biobase.

[Figure 3: Matrix band adaptation]
If there are no proximal contacts, a matrix system must be used before an adhesive build-up. There are many modern sectional matrix systems available, as well as the classic Tofflemire matrix with specific DME bands. In any case, it is important to ensure that the matrix is applied to the cavity edge with a tight seal and that there is good proximal contact to the neighbouring tooth (Fig.3).

[Figure 4: Pre endodontic build up complete]
If the pulp chamber has already been removed, or if root canal orifices are visible during restoration treatment, a sterilized Teflon film can be used as a placeholder in the pulp chamber. This will reliably prevent unintentional influx of composite into the pulp chamber. This is followed by the layer-by-layer reconstruction of the missing cavity walls with a composite resin restoration (Fig. 4).
To sum up so far: creating a pre-endodontic build-up is an important first step in carrying out effective endodontic treatment. Doing this paves the way for further treatment and allows:
Exactly the same care should be taken during pre-endodontic build-up as in all other steps of an endodontic treatment. Completion of this step fulfils the following objectives:
1. It prevents contamination of the root canal space by bacteria present in the carious lesions.
2. It prevents contamination of the canal space by oral fluids and saliva between appointments.
3. It allows the intracanal medicaments to function at their best. At the same time, the medicaments will not leach out into the oral cavity. This ensures that the root canal space remains in a medicated state between appointments.
4. It provides four good walls to enable the tooth to sustain the strength of a rubber dam clamp.
5. It is possible to re-establish a regular and stable contour of the tooth, to provide regular and easily locatable reference points to determine, with the use of rubber stops, the working length of the canals.
6. A meticulous pre-operative tooth build-up will reduce the possibility of a post-operative tooth fracture and improve the prognosis of the treatment.
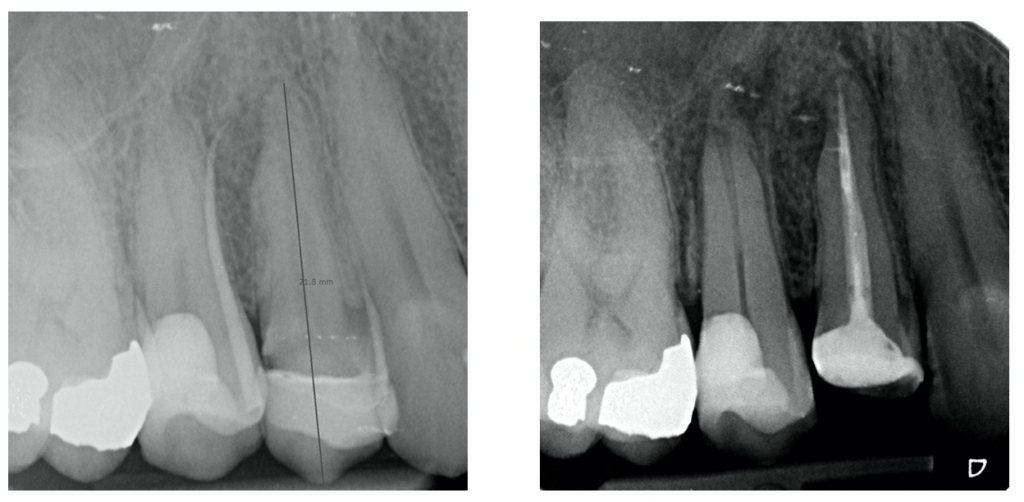
[Figure 5: Pre operative radiograph]
[Figure 6: Post operative radiograph]
Dhiraj summarises:“There are obvious benefits of this approach. It prepares the tooth well for endodontic treatment by protecting and stabilising it. It is also much more stable between appointments – with less likelihood of marginal leakage, fracture or dislodgment than a temporary material. However it can lengthen treatment time. Given the pros and cons, and the likelihood of more predictable patient outcomes due to early restorability assessment, it’s something I recommend as the very best patient care is always the ultimate goal.
Back to Blog
With practices in London and the South of England I am able to help your patients with dedicated and experienced endodontic care.
Read more

Aimed specifically at early career dentists, I can help with both the practical and patient care aspects of becoming a seriously good endodontist. Currently we have two courses running with dates set for 2023. Shake up your Shaping (1 day) and Endo Roots (3 days).
Read moreWe use cookies on our website. Some of them are essential, while others help us to improve this website and your experience.
Here you will find an overview of all cookies used. You can give your consent to whole categories or display further information and select certain cookies.
Essential cookies enable basic functions and are necessary for the proper function of the website.
| Name | |
|---|---|
| Provider | Owner of this website |
| Purpose | Saves the visitors preferences selected in the Cookie Box and other strictly functional behaviour of the web site |
| Host(s) | .evoendo.co.uk, evoendo.co.uk |
| Cookie Name | PHPSESSID,dmxlabs-kooke,cerber_groove,wordpress_* |
| Cookie Expiry | 1 Year |
Statistics cookies collect information anonymously. This information helps us to understand how our visitors use our website.
| Accept | |
|---|---|
| Name | |
| Provider | Google LLC |
| Purpose | Cookie by Google used for website analytics. Generates statistical data on how the visitor uses the website. |
| Privacy Policy | https://policies.google.com/privacy?hl=en |
| Cookie Name | _ga,_gat,_gid |
| Cookie Expiry | 2 Years |
| Accept | |
|---|---|
| Name | |
| Provider | |
| Purpose | Used to unblock Google Maps content. |
| Privacy Policy | https://policies.google.com/privacy?hl=en&gl=en |
| Host(s) | .google.com |
| Cookie Name | NID |
| Cookie Expiry | 6 Month |
| Accept | |
|---|---|
| Name | |
| Provider | |
| Purpose | Used to unblock Instagram content. |
| Privacy Policy | https://www.instagram.com/legal/privacy/ |
| Host(s) | .instagram.com |
| Cookie Name | pigeon_state |
| Cookie Expiry | Session |
| Accept | |
|---|---|
| Name | |
| Provider | Vimeo |
| Purpose | Collects information on the user's visits to the website, such as which pages have been read and offers best video quality based on determined visitor internet speed. |
| Privacy Policy | https://vimeo.com/privacy |
| Host(s) | .vimeocdn.com, fresnel.vimeocdn.com, player.vimeo.com |
| Cookie Name | vuid,sync_active,player |
| Cookie Expiry | 2 Years |
| Accept | |
|---|---|
| Name | |
| Provider | YouTube |
| Purpose | Used to unblock YouTube content. |
| Privacy Policy | https://policies.google.com/privacy?hl=en&gl=en |
| Host(s) | google.com |
| Cookie Name | NID,pref,VISITOR_INFO1_LIVE,CONSENT |
| Cookie Expiry | 6 Month |